Gastric Bypass Roux-en-Y
In recent years, better clinical understanding of procedures combining restrictive and malabsorptive approaches has increased the choices of effective weight loss surgery for thousands of patients. By adding malabsorption, food is delayed in mixing with bile and pancreatic juices that aid in the absorption of nutrients. The result is an early sense of fullness, combined with a sense of satisfaction that reduces the desire to eat.
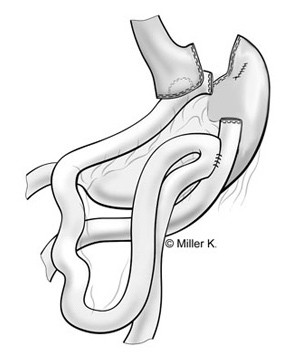
According to the American Society for Bariatric Surgery and the National Institutes of Health, Roux-en-Y gastric bypass is the current gold standard procedure for weight loss surgery. It is one of the most frequently performed weight loss procedures in the United States. In this procedure, stapling creates a small (15 to 20cc) stomach pouch. The remainder of the stomach is not removed, but is completely stapled shut and divided from the stomach pouch. The outlet from this newly formed pouch empties directly into the lower portion of the jejunum, thus bypassing calorie absorption. This is done by dividing the small intestine just beyond the duodenum for the purpose of bringing it up and constructing a connection with the newly formed stomach pouch. The other end is connected into the side of the Roux limb of the intestine creating the "Y" shape that gives the technique its name. The length of either segment of the intestine can be increased to produce lower or higher levels of malabsorption.
Advantages
-
The average excess weight loss after the Roux-en-Y procedure is generally higher in a compliant patient than with purely restrictive procedures.
-
One year after surgery, weight loss can average 77% of excess body weight.
-
Studies show that after 10 to 14 years, 50-60% of excess body weight loss has been maintained by some patients.
-
A 2000 study of 500 patients showed that 96% of certain associated health conditions studied (back pain, sleep apnea, high blood pressure, diabetes and
depression) were improved or resolved
Risks
-
Because the duodenum is bypassed, poor absorption of iron and calcium can result in the lowering of total body iron and a predisposition to iron deficiency
anemia. This is a particular concern for patients who experience chronic blood loss during excessive menstrual flow or bleeding hemorrhoids. Women, already at risk for osteoporosis that can
occur after menopause, should be aware of the potential for heightened bone calcium loss.
-
Bypassing the duodenum has caused metabolic bone disease in some patients, resulting in bone pain, loss of height, humped back and fractures of the ribs and
hip bones. All of the deficiencies mentioned above, however, can be managed through proper diet and vitamin supplements.
-
A chronic anemia due to Vitamin B12 deficiency may occur. The problem can usually be managed with Vitamin B12 pills or injections.
-
A condition known as "dumping syndrome " can occur as the result of rapid emptying of stomach contents into the small intestine. This is sometimes triggered
when too much sugar or large amounts of food are consumed. While generally not considered to be a serious risk to your health, the results can be extremely unpleasant and can include nausea,
weakness, sweating, faintness and, on occasion, diarrhea after eating. Some patients are unable to eat any form of sweets after surgery.
-
In some cases, the effectiveness of the procedure may be reduced if the stomach pouch is stretched and/or if it is initially left larger than
15-30cc.
-
The bypassed portion of the stomach, duodenum and segments of the small intestine cannot be easily visualized using X-ray or endoscopy if problems such as
ulcers, bleeding or malignancy should occur.
Frequently Asked Questions about Gastric Bypass Surgery
What is gastric bypass surgery?
Gastric bypass is a surgical method used to help people with morbid obesity lose weight and reverse other health problems associated with being overweight, such as high blood pressure and Type II diabetes. The Roux-en-Y gastric bypass, creates a small pouch in the top of the stomach to which the small intestine is connected. With a smaller stomach, the patient feels "full" sooner and is less likely to overeat. Depending upon what is best for each individual patient, the bypass is performed as an "open" procedure, or with a minimally invasive technique using laparoscopes.
Can anyone who is overweight have gastric bypass surgery?
The surgery is not a cosmetic procedure, but rather, a course of last resort for people who are at least 100 pounds over their ideal weight and have a body mass index (BMI) of over 40. Patients with a slightly lower BMI may be considered for the procedure if they have other obesity-related problems such as Type II diabetes, cardiovascular disease, or sleep apnea. Gastric bypass is also generally reserved for patients who have been unable to lose weight through weight reduction programs and exercise.
What are the risks of gastric bypass surgery?
As is true with any operation, there are complications associated with gastric bypass surgery. One of the most serious is leakage where the stomach pouch meets the small intestine.
With no treatment, approximately one in four gastric bypass patients will develop gallstones following surgery. That is why a bile thinning medication is prescribed after surgery.
Some other complications include abdominal hernia in open traditionally surgery, wound infection, and bowel obstruction. There is also the possibility of lung-related conditions, such as pulmonary embolism, and additional stress on the cardiac system; for these reasons, the patients are closely monitored during the post-surgical hospital stay. In very rare situations, a patient may even die as a result of the surgery or one of its complications.
Gastric bypass surgery reduces stomach capacity quite significantly. Does the stomach ever stretch back to a larger size?
Surgery reduces the stomach capacity by about 90 percent. Immediately after surgery, the pouch can hold approximately two ounces. Gradually, the stomach pouch does stretch somewhat and the capacity increases, but not to its original size.
How effective a procedure is the Roux-en-Y gastric bypass?
The results are very encouraging. But the surgery is not a magic "cure all" in itself: Eating healthy foods and exercising regularly are the other parts of the equation for success.
How long does recovery from gastric bypass surgery take?
Patients can expect to be out of bed by evening of the same day of the surgery, with a total hospitalization stay of about 4-6 days in our hospital. The surgical recovery period averages between 3-5 weeks.
How many pounds can someone expect to lose after surgery, and how long does it take to achieve the desired weight loss?
Every person's weight loss experience is different. As a rule of thumb, the heavier the patient, the more weight they are likely to lose. Most patients can expct to lose two-thirds of their excess weight. Most of that weight loss will occur within the first 12 months. That loss is almost always followed by a slight weight gain while the body is stabilizing, and is followed by another period of weight loss.
Losing the weight is only part of the picture, however. The difficulty can be in keeping it off. That is where gastric bypass surgery has proven to be so effective. Five years after surgery, 95% of all patients have maintained a loss of more than 50% of their excess weight. Keep in mind that on average, with a traditional diet-based weight loss program, only about 1% of morbidly obese persons maintain their weight loss at that level.
Do patients ever have to "diet" again following gastric bypass surgery?
The patient will have to adopt a healthy eating plan and an exercise program for the rest as well as vitamin suppliments of his or her life.
What is "dumping syndrome"?
When large amounts of high-calorie foods (especially those containing sugar) pass quickly from the stomach pouch into the intestine, fluid rushes into the small intestine to dilute the high concentration of sugar. The patient may feel faint, break out in a cold sweat, and have intestinal cramps followed by diarrhea. Fortunately, "dumping syndrome" can be averted simply by the patient avoiding high intakes of sweets.
What happens if someone "cheats" on the recommended post-surgical diet?
Usually, "cheating" cures itself, as the consequences can be quite uncomfortable for the patient. Eating high-calorie foods can bring on "dumping syndrome," which results in cold sweats, a feeling of faintness, intestinal cramps, and diarrhea. It is such an unpleasant experience that most people do not keep on "cheating."
How does gastric bypass surgery affect which medications a patient is able to take?
Patients should avoid aspirin or aspirin-containing medications and anti-inflammatory drugs; they can irritate the intestinal tract’s inner lining and sometimes cause ulcers. For the same reason, alcohol and tobacco products should be avoided, as well.
Is pregnancy possible following gastric bypass surgery?
Many obese women of childbearing age do not have menstrual periods, a condition known as amenorrhea, and thus, are unable to become pregnant. After the surgery and subsequent weight loss, regular menstrual cycles typically resume. Barring other fertility-related problems, these women are able to become pregnant. However, it is not advisable to attempt a pregnancy until 18 months after the surgery. Before then, the rapid weight loss and nutritional deficiencies can harm a developing fetus.
When the waiting period is over, these women–with proper pre-natal care and monitoring by their obstetrician and bariatric team–can go on to have uneventful pregnancies and healthy babies. Despite the reduced size of her stomach, the mother-to-be can still intake sufficient calories for both the fetus and herself.
If I want to pay for the surgery myself, in the event my insurance won't cover it, how much can I expect to pay?
If you are interested in paying out-of-pocket for the procedure, the fees at are in the approx. $ 7,000 to $ 12,000 range (depending upon the different operations and services needed) and are payable in full prior to the surgery
